In a previous study (SY Ahn et al, Cancer Res Treat 2023), we reported that the presence of only the basic leucine zipper in-frame mutation (bZIP in-f) CEBPA is associated with favorable outcomes in patients with CEBPAdouble mutations. However, when bZIP in-fCEBPAmutations were accompanied by certain mutations in chromatic/DNA modifiers, cohesion complex, and splicing genes, patients exhibited inferior overall survival (OS). FLT3-ITD or additional cytogenetic abnormalities is known to rarely co-occur with CEBPA mutation in patients with AML. In cases where both bZIP in-fCEBPA and FLT3-ITD coexist, there are conflicting aspects in risk stratification, and research on its prognostic significance is limited. Therefore, we aimed to evaluate the prognostic significances of the co-occurrence of bZIP in-fCEBPAmutation with unfavorable genetic abnormalities in acute myeloid leukemia.
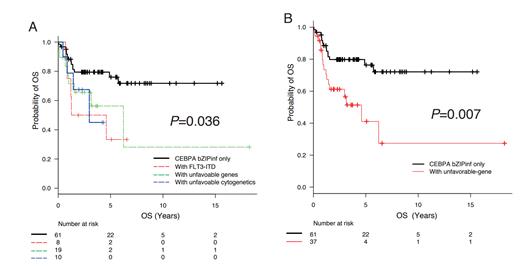
In 832 patients who were diagnosed with AML excluding acute promyelocytic leukemia and underwent intensive induction therapy, 98 (11.8%) had bZIP in-fCEBPA. Among 98 patients with bZIP in-fCEBPA, eight cases had FLT3-ITD (5 with low allelic ratio, 3 with high allelic ratio), 19 patients had unfavorable genetic mutations according to the 2022 European LeukemiaNet guidelines, and 10 patients had non-favorable cytogenetic abnormalities as detected in diagnostic samples. We observed no clinical differences in features such as age, sex, WBC count, bone marrow blast percentage at diagnosis based on the co-occurrence unfavorable genetic abnormalities (unfavorable-gene). Among the 98 patients with bZIP in-f CEBPA, 30 out of 37 patients with unfavorable-gene achieved complete remission (CR) after induction therapy, and 55 out of 61 without unfavorable genetic abnormalities showed CR (p=0.20). Allogeneic hematopoietic cell transplantation was proceeded at first CR in 21 out of 37 unfavorable-gene group, and 35 out of 61 bZIP in-fCEBPAonly group ( p=1.00). In the survival analysis, patients with FLT3-ITD, unfavorable genetic co-mutated, or non-favorable cytogenetic abnormalities with bZIP in-fCEBPA showed inferior OS (p=0.036) (Fig. A). Due to the limited number of patients for analysis, we classified them into two group: the unfavourable-gene group and bZIP in-fCEBPAonly group. We observed that the unfavourable-gene group had a poor OS compared to the bZIP in-fCEBPAonly group (HR 2.71, 95 CI; 1.32-5.55, p=0.007) (Fig.B). On multivariate analysis, unfavorable-gene group was only poorrisk factor for OS. Despite the inclusion of a relatively small number of patients, our study demonstrates that when co-occurrence of bZIP in-fCEBPA withunfavourable genetic abnormalities, it results in a poor prognosis. To confirm its clinical significance, further validation with a larger patient population is necessary.
Disclosures
Kim:Novartis: Consultancy, Honoraria, Research Funding; BMS: Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Paladin: Consultancy, Honoraria, Research Funding; Merk: Consultancy; Sanofi: Consultancy, Honoraria.